Introduction
Antimicrobial Resistance Statistics: Antimicrobial resistance (AMR) remains a critical global health challenge, eroding the effectiveness of antibiotics and other antimicrobial agents. As bacteria, viruses, fungi, and parasites increasingly develop resistance to existing treatments, infections become increasingly harder to control, leading to prolonged illnesses, higher medical costs, and higher mortality rates worldwide. The World Health Organization estimates that AMR is responsible for over 1 million deaths annually, with resistant infections spreading rapidly across regions and healthcare settings.
This growing threat is fueled by factors such as the overuse and misuse of antibiotics in human medicine and agriculture, inadequate infection prevention measures, and limited development of new antimicrobial drugs. Understanding the latest statistics on antimicrobial resistance (AMR) is essential for policymakers, healthcare professionals, and stakeholders to formulate effective strategies that can curb the rise of resistance and protect global health security.
Editor’s Choice
- An estimated 700,000 fatalities annually are attributed to infections resistant to antimicrobial drugs, with the highest burden observed in developing and middle-income nations.
- The most commonly resistant bacteria include critical pathogens such as Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, and Mycobacterium tuberculosis, posing significant treatment challenges.
- Excessive and inappropriate use of antibiotics across medical and agricultural sectors remains a key factor driving the rapid emergence and spread of antimicrobial resistance.
- Numerous regions lack adequate frameworks for monitoring antimicrobial resistance (AMR), resulting in insufficient data and difficulties in accurately assessing resistance patterns worldwide.
- Infections caused by resistant microorganisms prolong patient hospitalization by approximately 6.4 days and can elevate healthcare expenses by up to 60%, placing substantial pressure on healthcare systems.
- The World Health Organisation’s Global Action Plan on AMR focuses on enhancing public education, bolstering surveillance mechanisms, and promoting prudent antibiotic stewardship to curb the growth of resistance.
Global Antibiotics Market Size
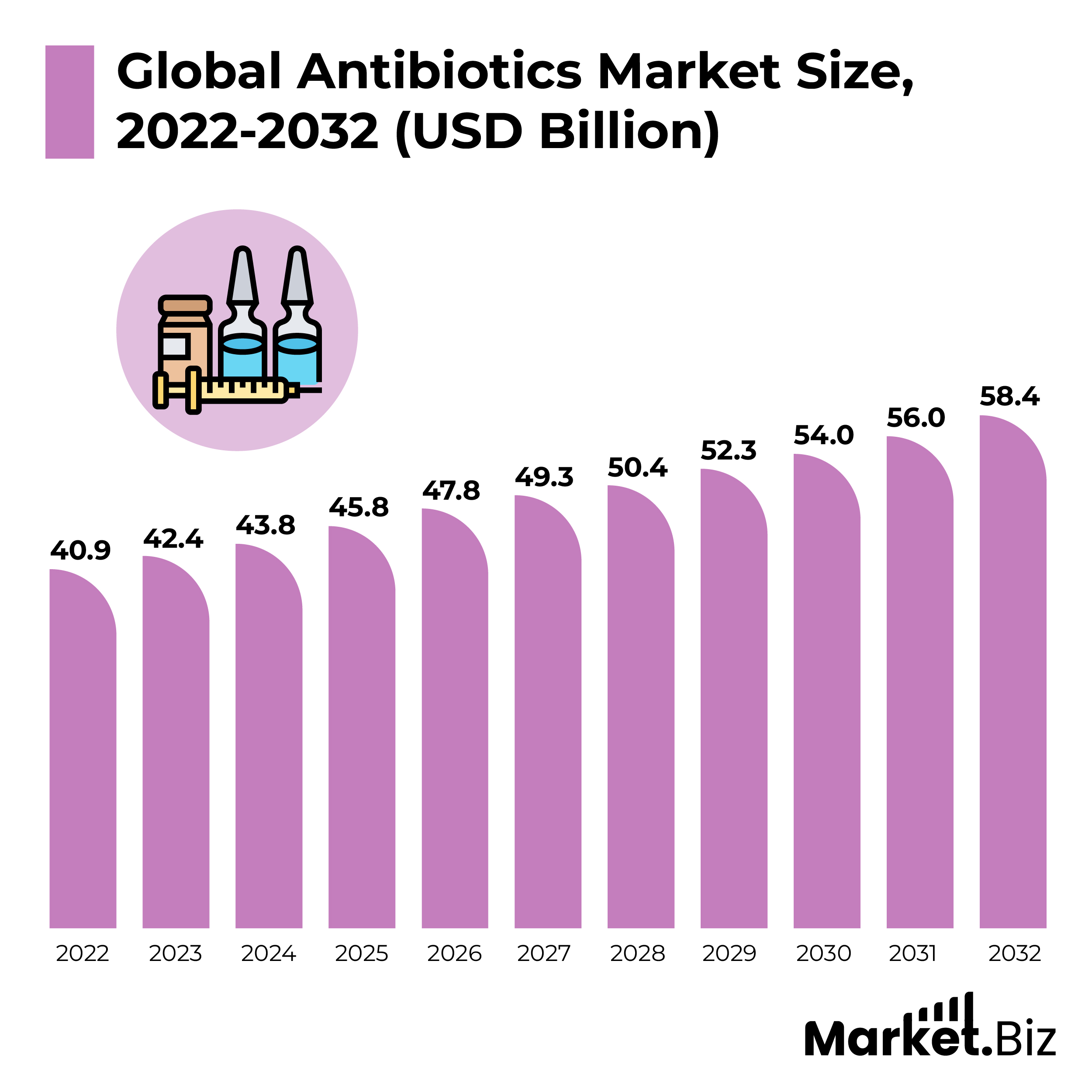
- According to Market.us, the global antibiotics market is projected to grow from $45.8 billion in 2025 to $58.4 billion by 2032, representing a compound annual growth rate (CAGR) of 3.7% from 2022 to 2032.
- The market’s expansion is primarily driven by the rising incidence of infectious diseases, an ageing population, and increased awareness, along with enhanced access to healthcare services.
- In 2022, the penicillin segment captured the largest revenue share of 24.5%, driven by its extensive use in treating bacterial infections such as bronchitis, pharyngitis, and skin ailments. Moreover, the growing adoption of penicillin across both developed and emerging markets is expected to sustain its market dominance.
- The respiratory infections segment led the market in 2022 due to the high patient population suffering from respiratory conditions. Factors such as escalating global pollution levels and climate change have significantly increased respiratory health issues. Additionally, the COVID-19 pandemic’s impact on respiratory health has further fueled growth in this segment.
- The parenteral antibiotics segment commanded the largest revenue share in 2022, driven by the steady increase in global inpatient hospital admissions. Advances in technology, coupled with efficient dosing through syringes, have significantly boosted demand for this administration route.
- Broad-spectrum antibiotics are projected to secure the largest revenue share in 2022, as they effectively target both gram-positive and gram-negative bacteria. Their ability to address a wide range of infections also aids in combating antimicrobial resistance, making them highly favored for treatment.
- Hospital pharmacies dominated the market, accounting for a 28% revenue share in 2022 due to patients’ preference for receiving treatment within hospital settings. The availability of trained healthcare professionals in these facilities has also contributed to market growth.
- North America accounted for 32% of the market revenue in 2022, driven by the increasing burden of infectious diseases and substantial government healthcare spending.
(Source: Market.us)
Global Prevalence of Antimicrobial Resistance
Antimicrobial resistance (AMR) is intensifying globally, creating major obstacles in the effective management of bacterial infections. The distribution of resistant pathogens varies significantly across different regions and bacterial species, with developing countries experiencing notably higher prevalence rates.
- .In numerous countries, resistance of Escherichia coli to fluoroquinolone antibiotics—a widely used antibiotic class has soared up to 82%, raising substantial treatment concerns.
- Over 50% of Klebsiella pneumoniae infections in certain areas exhibit resistance to third-generation cephalosporins, which are crucial antibiotics for treating severe bacterial infections.
- Approximately 3.4% of patients previously treated for tuberculosis are affected by multidrug-resistant tuberculosis (MDR-TB), underscoring ongoing difficulties in tuberculosis control.
- Carbapenem-resistant Enterobacteriaceae (CRE) have been detected globally within healthcare facilities, with prevalence rates varying from below 1% to more than 50%, depending on the country.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections occur in both medical institutions and the community, with rates ranging widely from under 1% to above 50% in different countries.
- Vancomycin-resistant Enterococcus (VRE) has been identified in various parts of the world, with prevalence ranging from less than 1% to over 60%.
- Low- and middle-income countries bear a disproportionate share of the AMR burden, primarily due to limited healthcare availability and the misuse of antibiotics.
- In these regions, up to 90% of Escherichia coli strains causing urinary tract and bloodstream infections are resistant to commonly administered antibiotics.
- MRSA prevalence surpassing 50% has been reported in select healthcare settings of developing countries, indicating severe infection control challenges.
- CRE infection rates in hospitals from some Asian and Mediterranean countries exceed 50%, highlighting an urgent need for effective containment strategies.
- CRE infections carry high fatality rates, with studies reporting mortality between 40% and over 50%.
(Source: World Health Organization)
Healthcare-associated and Community-Acquired Infections
Healthcare-associated infections (HAIs) and infections acquired in community settings continue to represent a significant public health challenge worldwide. Both hospital environments and outpatient care significantly contribute to the burden of antibiotic-resistant infections, underscoring the critical need for enhanced infection control and responsible antibiotic use.
- In developed nations, between 7% and 10% of hospitalized patients contract at least one healthcare-associated infection during their stay, reflecting the persistent risk within clinical settings.
- In the United States, data indicate that approximately one in every 31 hospitalized individuals has an active healthcare-associated infection at any given moment, highlighting the widespread nature of these infections.
- Methicillin-resistant Staphylococcus aureus (MRSA) remains a prevalent, drug-resistant pathogen primarily associated with hospital environments.
- Annually, in the U.S., invasive MRSA infections affect around 80,461 individuals, resulting in an estimated 11,285 fatalities, illustrating the severe outcomes associated with this resistant bacterium.
- Carbapenem-resistant Enterobacteriaceae (CRE) infections also pose a grave threat, with about 13,100 cases reported each year in the U.S., contributing to approximately 1,100 deaths.
- Clostridioides difficile infection (CDI) is notably common in healthcare settings, especially following antibiotic therapy, and is a leading cause of hospital-acquired diarrhoea.
- The U.S. reports nearly 223,900 CDI cases annually, with deaths reaching around 12,800, emphasizing the infection’s serious health impact.
- Community healthcare settings, including primary care and outpatient clinics, account for up to 90% of total antibiotic consumption in some countries, signaling a critical area for stewardship.
- In the U.S. outpatient sector, approximately 30% of prescribed antibiotics are considered unnecessary, indicating a significant opportunity to reduce inappropriate antibiotic use.
(Source: World Health Organization, Center for Disease Control and Prevention)
Consequences of Antimicrobial Resistance
Antimicrobial resistance (AMR) continues to pose a profound threat to public health, significantly affecting patient outcomes, healthcare costs, and mortality worldwide. The growing prevalence of drug-resistant infections undermines treatment efficacy and places immense strain on healthcare systems globally. Below are critical insights into the impact of AMR across various domains:
Healthcare-Associated Infections (HAIs)
- Globally, drug-resistant healthcare-associated infections are responsible for approximately 700,000 deaths each year.
- In the United States, nearly 2 million individuals contract HAIs annually, resulting in about 99,000 fatalities.
- At any given time, an estimated 1 in 31 hospitalized patients in the U.S. suffers from at least one healthcare-associated infection.
- Europe experiences roughly 4.2 million cases of HAIs annually, with around 37,000 deaths directly linked to these infections.
(Sources: WHO, ECDC)
Rising Treatment Failures
- Antibiotic treatment failure rates for urinary tract infections caused by Escherichia coli climbed from 5.7% in 2011 to 13.9% in 2017.
- Multi-drug-resistant bacteria are responsible for about 60% of urinary tract infections globally.
- For community-acquired pneumonia caused by Streptococcus pneumoniae, treatment failure rates range from 17% to 26%, primarily driven by resistance.
- Resistance to at least one standard antibiotic has been reported in approximately 81% of countries for gonorrhea infections.
- The success rate for treating multidrug-resistant tuberculosis (MDR-TB) remains low at around 57%, compared to higher rates for drug-sensitive forms.
(Sources: CDC, WHO)
Escalating Economic Burden
- The worldwide economic toll of AMR could reach between $2 trillion and $100 trillion by 2050 if not effectively managed.
- In affluent countries, costs related to AMR infections may account for 2–3% of their GDP.
- The U.S. faces an estimated annual direct healthcare expenditure of US$20 billion for antibiotic-resistant infections.
- Hospital stays for resistant infections in the U.S. average approximately $ 34,000 per patient, which is approximately 1.5 times more costly than for non-resistant cases.
- In the European Union, AMR-related healthcare expenses amount to around €1.5 billion annually, with total costs, including productivity losses, reaching €7.1 billion.
- Low- and middle-income countries face a severe economic impact, with projections indicating that AMR could drive up to 28.3 million people into extreme poverty by 2050.
(Sources: European Commission, Review on Antimicrobial Resistance, CDC, World Bank)
Mortality Attributable to AMR
- Without intervention, drug-resistant infections are projected to cause up to 10 million deaths annually by 2050.
- In Europe, AMR accounts for approximately 33,000 deaths each year.
- In the U.S., drug-resistant infections contribute to over 35,000 deaths annually.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections alone result in an estimated 10,000 deaths annually in the United States.
- Worldwide, multidrug-resistant tuberculosis causes roughly 240,000 deaths each year.
(Sources: CDC, WHO)
Key Drivers Behind Antimicrobial Resistance: An In-Depth Analysis
The surge in antimicrobial resistance (AMR) is fueled by a complex interplay of factors spanning healthcare practices, agriculture, environmental conditions, and global movement. Understanding these contributing elements is crucial for formulating effective strategies to curb resistance and protect public health worldwide.
Misuse and Overprescription of Antibiotics
- Worldwide antibiotic intake reached an estimated 34.8 billion defined daily doses (DDD), averaging 21.1 DDD per 1,000 inhabitants annually.
- Intake rates vary drastically, with some countries reporting less than 10 DDD per 1,000 people per day, while others exceed 60 DDD.
- In affluent nations, between 20% and 50% of outpatient antibiotic prescriptions are deemed unnecessary.
- A systematic review highlighted that globally, approximately 52% of antibiotic prescriptions in main care are inappropriate, with prevalence reaching from 8% to 100% depending on the region and study.
- Research across 36 countries revealed a median of 32% of antibiotic purchases occur without a prescription, with figures reaching from 4% to 77%.
- In low- and middle-income countries, access to antibiotics without a formal prescription often surpasses 50%, exacerbating misuse.
(Sources: The Lancet Infectious Diseases, BMJ Global Health, PLoS ONE)
Antibiotic Use in Agriculture
- Nearly 73% of the world’s antimicrobial agents are utilized in animal farming, primarily to promote growth and prevent disease.
- In countries such as the U.S. and China, over half of all antimicrobials produced are consumed within livestock industries.
(Source: WHO)
Weak Healthcare Infrastructure
- In low- and middle-income regions, hand hygiene compliance among healthcare professionals is often below 50%, undermining infection control.
- Only 28% of African healthcare facilities have access to basic water services, while 19% lack sanitation altogether.
- Access to clinical microbiology laboratories and antibiotic susceptibility testing remains limited, with only 34% and 15% availability, respectively, in low-income countries.
- In sub-Saharan Africa, just 20% of countries maintain national antimicrobial resistance surveillance systems.
- Physician density in sub-Saharan Africa averages 2.6 per 10,000 people, far below the global mean of 15.1 per 10,000.
(Sources: World Health Organization)
Insufficient Admission to Clean Water and Sanitation
- About 2.2 billion people global lack access to safely managed drinking water.
- Approximately 4.2 billion individuals lack admission to safely achieved sanitation facilities.
- Poor water and sanitation conditions contribute to an estimated 800,000 deaths annually from diarrheal illnesses.
(Source: WHO)
Impact of Global Migration and Travel
- Travellers are more likely than non-travellers to carry multidrug-resistant bacteria, with prevalence ranging from 2% up to 50%, influenced by destination and exposure risks.
- The chance of acquiring resistant infections increases by an estimated 20% to 30% during international travel.
- Genetic studies of MRSA strains suggest that global travel accounts for 20% to 50% of transmission events worldwide.
- Each year, over 200 million global travellers face the risk of acquiring drug-resistant infections during their journeys.
(Sources: Journal of Travel Medicine, The Lancet Infectious Diseases)
Key Strategies to Combat the Rising Threat of Antimicrobial Resistance
Combating antimicrobial resistance (AMR) demands comprehensive and coordinated efforts that focus on optimizing antibiotic use, enhancing diagnostic accuracy, and expanding preventive vaccination coverage. These targeted strategies have proven effective in reducing the misuse of antibiotics and slowing the spread of resistant infections.
Antibiotic Stewardship Programs
- Introducing stewardship initiatives within healthcare institutions has been shown to lower inappropriate antibiotic prescribing by 20% to 50%.
- Evidence from large U.S. hospitals indicates a 47% reduction in broad-spectrum antibiotic consumption following the rollout of stewardship protocols.
- Financial analyses suggest that stewardship programs in major teaching hospitals can yield annual savings close to $900,000, reflecting both clinical and economic benefits.
(Source: American Journal of Health-System Pharmacy)
Immunization and Vaccination Initiatives
- In the United States, the introduction of the 7-valent pneumococcal conjugate vaccine (PCV7) has been widely adopted for children under the age of five.
- The newer PCV13 vaccine has contributed significantly to lowering antibiotic resistance rates associated with invasive pneumococcal diseases worldwide.
- Research from Kenya showed a remarkable 72% reduction in invasive Haemophilus influenzae type b (Hib) disease following the introduction of the vaccine.
- A systematic review estimated that influenza vaccination can reduce antibiotic prescriptions by around 28% during flu seasons, underscoring its role in AMR prevention.
(Source: The Lancet Infectious Diseases)
Enhanced Diagnostic Testing
- The adoption of rapid diagnostic tools can decrease unnecessary antibiotic prescriptions by 20% to 50%, allowing for more precise and timely treatment decisions.
- A study conducted at a pediatric hospital in the United States found that rapid diagnostics for bloodstream infections led to a 54% reduction in the use of broad-spectrum antibiotics.
(Source: JAMA)
Recent Developments
Investment in Antimicrobial Research Initiatives
- Government bodies have allocated substantial funds to support research and development aimed at discovering new antibiotics and innovative diagnostic tools to tackle antimicrobial resistance.
- Non-governmental organizations and charities have secured grants and donations to finance projects focused on antimicrobial stewardship, infection prevention, and public health strategies aimed at combating drug-resistant pathogens.
Worldwide Surveillance and Data Sharing on AMR
- Global surveillance networks actively track trends in antimicrobial resistance, providing critical data that shapes public health policies and guides clinicians in antibiotic prescribing decisions.
- Joint international efforts focus on harmonizing surveillance techniques and establishing uniform reporting frameworks, enabling seamless data exchange and comprehensive analysis across nations and regions.
Public Awareness and Educational Campaigns
- Health authorities have launched targeted awareness campaigns to educate healthcare professionals and the general public about the responsible use of antibiotics and infection control measures.
- Specialized training programs are designed for medical practitioners, veterinarians, and those involved in agriculture to promote prudent antimicrobial use across the human health, animal care, and farming sectors.
Antimicrobial Stewardship Implementation in Healthcare
- Medical institutions have adopted stewardship programs designed to enhance antibiotic prescribing accuracy, minimize unnecessary antibiotic use, and prevent the development of resistant infections.
- Comprehensive guidelines and standardized protocols have been developed for effective stewardship across various healthcare settings, including hospitals, long-term care facilities, and outpatient clinics, ensuring consistent practices and monitoring.
Conclusion
Antimicrobial resistance stands as one of the most urgent global health threats today, severely compromising the effectiveness of vital antibiotics and other antimicrobial treatments. The rising incidence of resistant infections contributes to higher rates of illness, death, and healthcare expenses around the world. Tackling this issue demands a unified, multi-disciplinary effort focused on responsible antibiotic use, comprehensive surveillance, increased funding for research and innovation, and widespread education for both the public and healthcare professionals.
Key measures, such as reinforcing antimicrobial stewardship programs, improving diagnostic technologies, and expanding vaccination efforts, are essential to curb the spread of resistance. Without prompt and continuous intervention, antimicrobial resistance will escalate, putting at risk the progress made in modern medicine and global health.
FAQ’s
Antimicrobial resistance happens when bacteria, viruses, fungi, or parasites change in ways that reduce or eliminate the effectiveness of medicines designed to eliminate them, making infections more difficult to treat.
AMR is a worldwide problem impacting every nation, with resistant infections responsible for hundreds of thousands of deaths each year. The burden is especially high in low- and middle-income countries due to factors like limited access to healthcare.
The primary resistant bacteria include Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus (including MRSA), Enterococcus species, and Mycobacterium tuberculosis strains resistant to multiple drugs (MDR-TB).
The primary drivers of AMR are the excessive and improper use of antibiotics in humans and animals, inadequate infection prevention practices, poor sanitation, and limited access to rapid diagnostic tests.
AMR results in prolonged hospitalizations, escalated healthcare costs, increased rates of illness and death, and imposes significant pressure on healthcare infrastructure worldwide.
